Does the Court have jurisdiction over compliance with the Pre-Action Protocol for Low Value RTA Claims (“the Protocol”)? In its decision of 24 June 2025, the Court of Appeal decided in MH Site Maintenance Services Limited and another v James Watson [2025] EWCA Civ 775 that, when proceedings have been issued, the answer is “yes.”…
‘Back in the day’ – not a phrase ever used back in the day – I recall mention in pupillage of three occupational conditions, farmer’s lung, bird fancier’s lung and bagpiper’s lung. They acquired a sort of mythological status as no such cases ever passed across the desks of my pupil supervisors.
Farmer’s lung was first reported in 1713 and it came to be recognised as a condition in dairy farm workers handling mouldy hay. Bird fanciers were exposed to proteins, be it from the feathers or droppings of the pigeons they kept. Players of the pipes were caused to inhale fungal spores which, by dint of irregular cleaning, colonised the bag of the instrument.
In the event, all involved manifestations, or variants of, hypersensitivity pneumonitis [‘HP’]. This blog is prompted by seeing, in recent years, a distinct uptick in such claims and the recent publication of guidelines associated with the diagnosis and management of the condition. Even with effective management, in the context of personal injury claims, it is capable of being generative of high-value claims.
The Condition
HP, also known as extrinsic allergic alveolitis [‘EAA’], is caused by repeated inhalation of non-human protein, which can be of natural plant or animal origin or can be the result of a chemical conjugated to a human airway protein, such as albumin.
These substances trigger the immune system and cause short or long-term inflammation in the lungs. The inflammation of HP manifests itself in the alveoli and distal bronchioles. These inflammations prevent the lungs from working properly and can make it harder to breathe. Whereas some types of hypersensitivity pneumonitis can be treated by avoiding the substance that is causing the condition or with medicines, untreated, hypersensitivity pneumonitis can cause permanent, disabling and indeed life-limiting damage to the lungs.
Historically, HP has been categorised as acute, subacute, or chronic, depending on the frequency, duration, and intensity of exposure and the duration of illness. However, these categories are not easily separated.
The American Thoracic Society, the Japanese Respiratory Society, and Latin American Thoracic Association (Asociación Latinoamericana del Tórax) diagnostic guidelines in adults were collaboratively published in 2020 [‘the ATS guidelines’]. They classify patients as having fibrotic or non-fibrotic HP. Classification is determined by the predominant presence or absence of fibrosis on radiological and/or histopathological examination. The full text of the ATS/JRS/ALAT paper is available online here.
The year following, in 2021, the American College of Chest Physicians published its own set of guidelines. The full text is accessible here.
Both sets of guidelines were then the subject of a very interesting commentary, commended to all occupational disease practitioners, by Mark Hamblin, Helmut Prosch, Martina Vašáková in a peer-review paper entitled “Diagnosis, course and management of hypersensitivity pneumonitis” published in the European Respiratory Review 2022 31: 210169, for which the link is here.
What the last-mentioned paper concludes is that “making a diagnosis of HP can be challenging as its clinical, radiologic and histopathologic features overlap with those of other interstitial lung disease and it may not be possible to identify a culprit exposure”.
Causation of the Condition
This last observation points to the truth, on the present state of knowledge, that if diagnosis is challenging, proof of causation is the more so. In this connection, it perhaps suffices to draw out two aspects given emphasis in the ATS guidelines on 2020.
First, there is statement that “… the antigen and exposure are not identified in up to 60% of patients with HP, despite a thorough history and the significance of the positive antibody tests” (see page 38). Secondly, and allied to that first point, there is the statement that “a positive serum IgG result does not mean that the exposure is the cause of the lung condition; it only indicates that the patient has likely been exposed to a potential cause of HP at some point in his or her life, and it may be worthy of further consideration to explore the source of the potential causative agent in the patient’s domestic, social, and/or work environment” (see page 53).
On that basis, it will be readily understood, particularly with that 60% in mind, what challenges face claimants in establishing their cases ‘on a balance of probabilities’.
Another peer-reviewed paper worth having in mind, published a decade before Hamblin et al is “Hypersensitivity pneumonitis: insights in diagnosis and pathobiology” by Moisés Selman et al and found, in full, here. What this identifies is that over many years, the home slowly emerged as the primary causative environment from exposures to ordinary antigens under common living conditions in individual cases, rather than reports of large outbreaks. New sources of airborne organic particles are recognized every year.
Moreover, it reports on “An important study highlights the importance of occult exposure as a cause of disease and the ability of Hypersensitivity Pneumonitis to mimic Idiopathic Pulmonary Fibrosis (another interstitial lung disease). In that study, 60 consecutive patients diagnosed with diagnosis of IPF were prospectively followed up for 6 years. Almost half of the patients were subsequently diagnosed with chronic HP, and most of these cases were attributed to exposure to occult avian antigens from commonly used feather bedding. Pigeons, parakeets, budgerigars, and other small cage birds are usually involved, but the disease may also occur in individuals using featherdown duvets and pillows and even by indirect contact to birds in consorts (e.g., handling others’ clothing).”
What this points to is not only the complexity of the condition but once more the difficulties in establishing that the facts and matters that may be complained of, whether in the context of an occupational disease claim or one brought, say, by a tenant against a landlord for alleged mould are in fact causative at all.
Occupational Culprits
Certain occupations are implicated. Thus, hypersensitivity pneumonitis includes conditions such as farmers’ lung and mushroom workers’ lung. Several fungal and bacterial components of organic dusts have been specifically linked with hypersensitivity pneumonitis.
Next, the ‘Systematic Review of Systematic Review: Occupational illness in the waste and recycling sector’ authored by Poole and Basu in 2017 (and published Occupational Medicine 2017;67:626-636) found a “few case reports of allergic disease such as extrinsic allergic alveolitis (hypersensitivity pneumonitis), allergic bronchopulmonary aspergillosis and occupational asthma”. What is thought apparent is that a distinction falls to be drawn between those exposed to aerosols from the waste management industry, which should not be conflated with or readily extended to ordinary refuse and street cleaning.
The year following, in 2018, the Health and Safety executive, Annual Science Review, recorded that, by reference to all cases of occupational HP reported to the Surveillance of Work-related and Occupational Respiratory Disease [‘SWORD’] scheme between January 1996 and December 2015, the most reported causative agents were metalworking fluids.
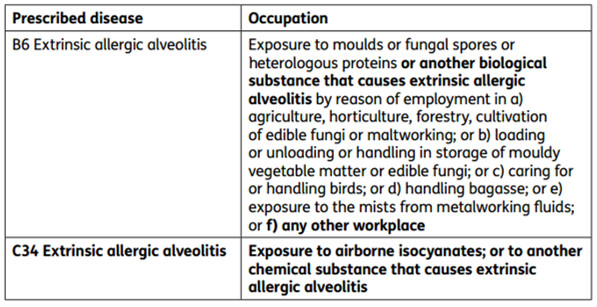
In regard to prescription of disease relevant to HP/EAA by the Industrial Injuries Advisory Council [‘IIAC’], EAA has been a prescribed disease since 1964 when farmer’s lung due to “exposure to the dust of mouldy hay or other mouldy vegetable produce” was scheduled. The terms of prescription were extended in 1983 to include a list of other well-established causal agents, and in 2006 to include cases caused by contaminated metalworking fluid. All of this is set out at para 16 of the IIAC report published a decade later into ‘Extrinsic allergic alveolitis: isocyanates and other occupational causes’ (published 12 April 2016 and accessible from this link). Given that isocyanates are chemical and not biological agents, the IIAC’s report created a new ‘C’ (i.e. chemical) disease section within the prescription schedule and enlarged the ‘B’ (i.e. biological) section as set out in the table below:
What this points to is that, whilst relatively rare, the condition is sufficiently serious in its effects to be the subject of active, ongoing research not only in the field of occasional hygiene but, anterior to that, medically. By way of one example, ‘Diagnosis of Fibrotic Hypersensitivity Pneumonitis: Is There a Role for Biomarkers?’, by Pereira et al points to advances in diagnostic techniques, albeit resolving the issue of causation remains.
Practitioners’ Tips
Noting those different categories of acute, sub-acute, or chronic, as ever, building a chronology is key. That exercise will necessarily be informed by a close questionnaire by Part 18 request of the kind that might be administered in a clinical questionnaire. Those questions will in turn necessarily be informed by what the medical records disclose – in my experience, sub-plots relating to alternative causes than the one asserted can and do feature in these cases.
The starting (and possible end) point will be what the chest physicians have to report. In my experience of these cases, less reliance has been placed on the chest radiograph appearances in hypersensitivity pneumonitis since at least CT scanning became widespread.
Irrespective of the cause, the radiological features of HP/EAA are similar, but vary depending on the phase of the disease. Acute EAA is usually self-limiting and is therefore unusual for imaging. In the subacute phase the chest radiograph commonly shows ground-glass opacification or fine nodularity involving the mid or lower zones of the lung (see Barber C, Hansell DM, McSharry CP. Extrinsic Allergic Alveolitis. In: Parkes’ Occupational Lung Disorders, 4th ed., 2017). In the acute HP, a variety of distributions has been described. Put another way, none of these findings are specific to HP. Indeed, up to 20% of individuals with acute HP have normal chest x-rays (see Lacasse Y, Cormier Y. Hypersensitivity pneumonitis. Orphanet J Rare Dis. 2006; 1:25).
It is difficult to envisage a case which will not represent a significant area of contention, even assuming breach and medical and legal causation are established. Whether in their bringing or their defence, claims of alleged HP/EAA provide a quintessential example of how the devil is in the detail.
Recent Posts
In the recent Judgment of Edwards and ors v 2 Sisters Food Group Limited [2025] EWHC 1312 (KB), Sir Peter Lane considered causation in work-related COVID-19 claims and the courts’ approach to a summary judgment application where further evidence may yet be adduced by the respondent. This Judgment is of significance for anyone dealing with…
Philip Turton adds to his article on URS Corporation Limited v BDW Trading Limited. This article can be read here. Two weeks ago I wrote about the effect of URS Corporation Limited v BDW Trading Limited [2025] UKSC 21 (“URS Corporation”) on claims for contribution in mesothelioma cases. The effect of the decision in the…

